
Your doctor can help you understand what devices should be avoided.
#FAILURE TO CAPTURE PACEMAKER TV#
These do not include simple, everyday devices such as cell phones, microwaves, electric blankets, or TV remotes. There is electromagnetic interference caused by strong magnets or power generators.Doctors will use that data to adjust your pacemaker to work most effectively for you.

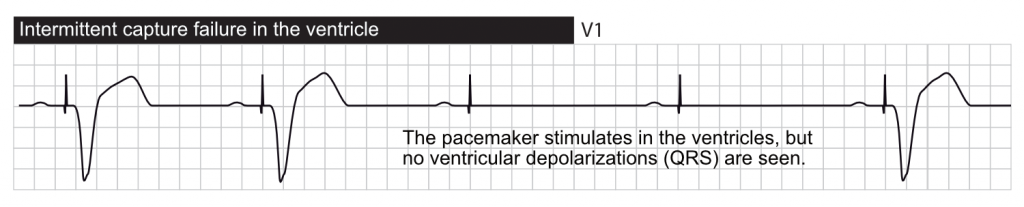
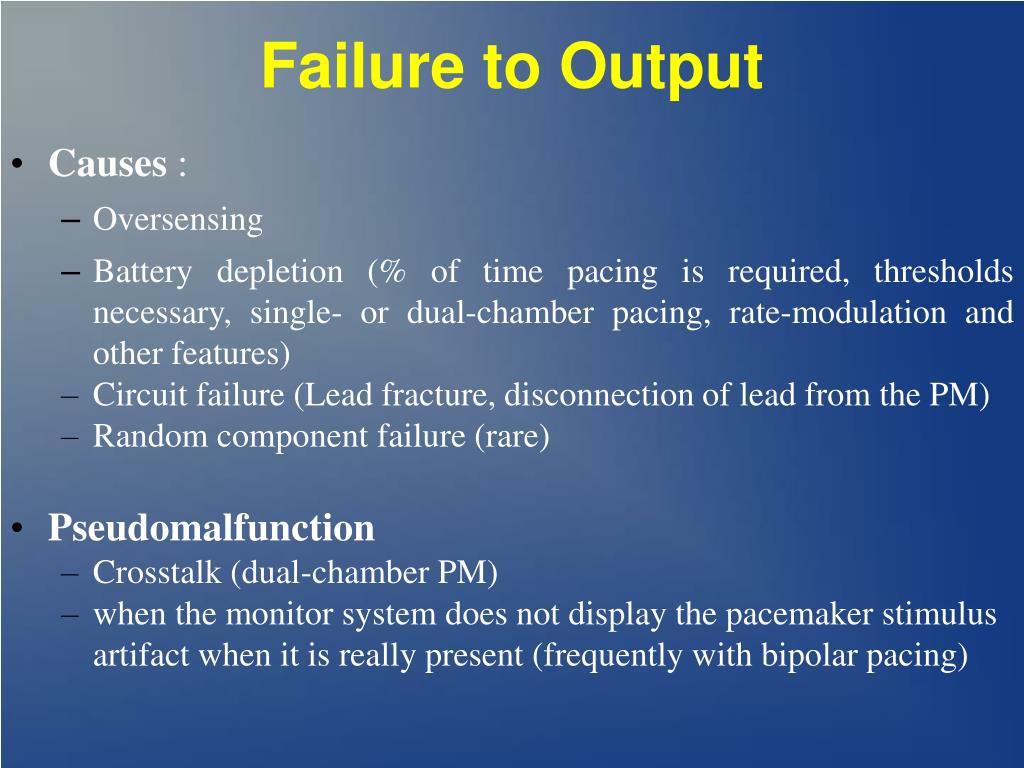
Your pacemaker records your heart’s electrical activity. Your condition has changed and it needs to be reprogrammed.There are several reasons why your pacemaker might stop working. You might have chest pain, difficulty breathing, dizziness, or lightheadedness. You can tell if your pacemaker is malfunctioning if you are starting to experience symptoms of arrhythmia. Signs and Causes of Pacemaker Malfunction These pulses travel through the wires to the heart, helping the heart adjust its rhythm.
#FAILURE TO CAPTURE PACEMAKER GENERATOR#
If the electrode detects an abnormal heartbeat, the computer tells the generator to create electrical pulses. The electrodes transmit this data through wires to a computerized, battery-powered generator. Pacemakers consist of electrodes that monitor your heartbeat. To avoid this, a pacemaker is used to correct abnormal heart rhythms. People with these conditions can struggle with getting enough blood pumped through the body, causing tiredness, difficulty breathing, or even fainting. This includes tachycardia, which is an unusually fast heart rate, and bradycardia, which is an unusually slow heart rate. How Your Pacemaker Helps Your HeartĪ pacemaker helps people with arrythmias. These devices are essential to patient health, so it is important to know if your pacemaker has stopped working and what to do about it. There are 3 million people living with pacemakers around the world, and 600,000 new pacemakers are implanted each year. Electrophysiology Study: How EP Doctors Diagnose AFibĪ pacemaker is a device placed in your chest or abdomen that sends electrical pulses, helping the heart to beat at a normal rhythm.Toxicity in these patients may present with pacemaker ventricular capture latency or failure to capture. The flecainide level drawn on arrival was 3.09 mcg/mL.ĬONCLUSIONS: Flecainide increases the ventricular capture threshold for pacemakers. After multiple boluses of IV sodium bicarbonate, the QRS acutely narrowed, latency interval improved, and consistent pacing capture was achieved. The pacemaker was interrogated, revealing a significant increase in ventricular threshold from 0.75 V at 0.5 ms at baseline to 5.0 V at 1 ms to obtain consistent capture. A 12-lead ECG demonstrated atrial and ventricular pacing with severely widened QRS complex and a significant latency between the pacemaker ventricular spike and the ventricular capture. Lab work was notable for creatinine at 2.12 mg/dL. She was found to be hypotensive and bradycardic, with a heart rate between 30 to 40 beats per minute.

We describe a unique case of flecainide toxicity secondary to acute kidney injury in the setting of a dual-chamber pacemaker, resulting in ventricular capture latency and intermittent failure to capture.ĬASE REPORT: The patient was a 91-year-old female with a history of atrial fibrillation maintained in sinus rhythm on flecainide, who presented complaining of purple visual disturbances and syncope. It is associated with a potent adverse effect profile however, the effects of flecainide toxicity in the setting of a pacemaker have not been well described. BACKGROUND: Flecainide is a class Ic antiarrhythmic agent used in the treatment of supraventricular and ventricular arrhythmias.


 0 kommentar(er)
0 kommentar(er)
